Climate action in healthcare
Climate change seems like a distant issue, until it shows up in your backyard.
Well, last week, it landed in mine.
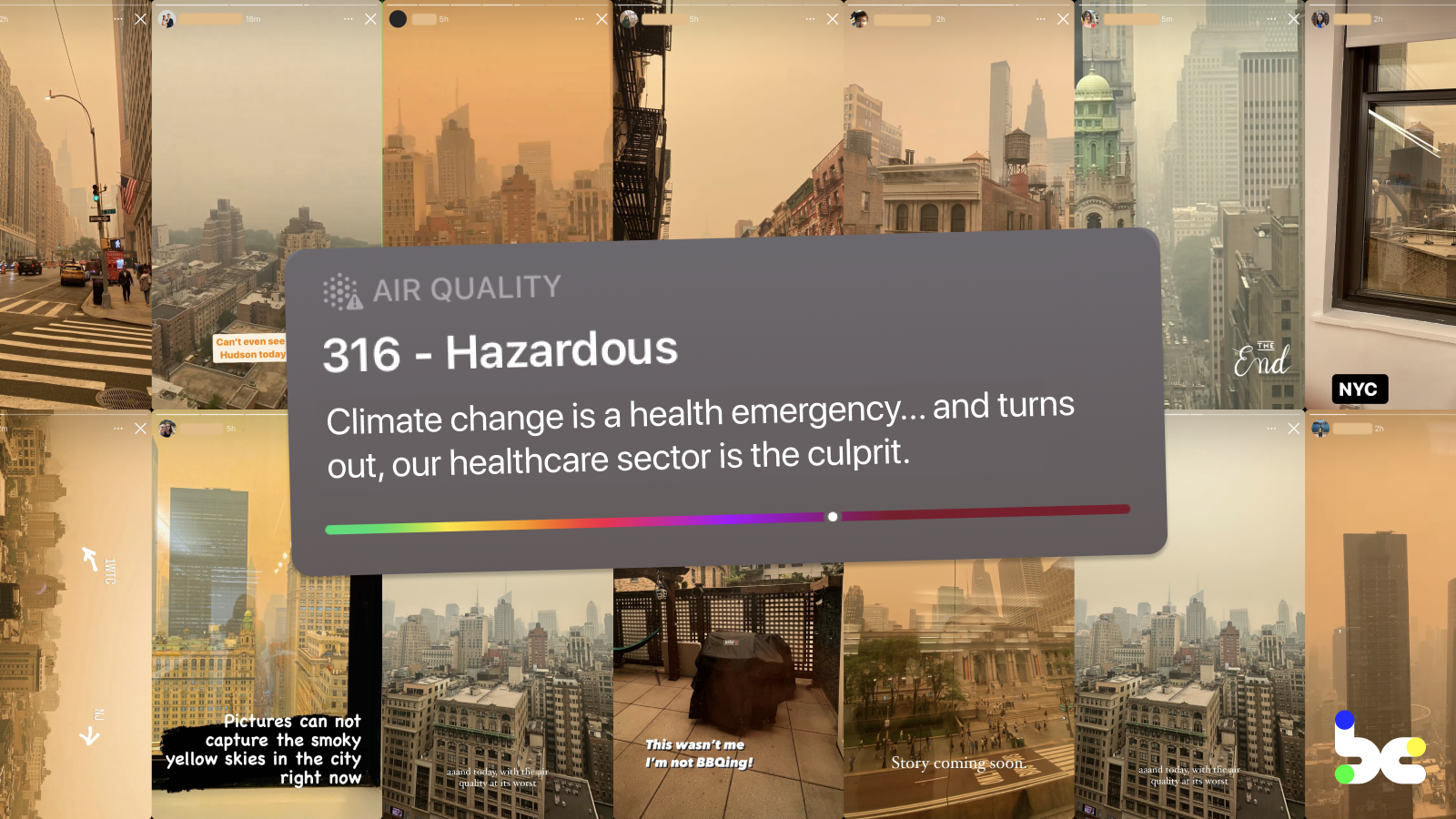
My Instagram stories were filled with New York City covered in a hazy orange smog, selfies taken in N95s, and screenshots of the AQI going up and up (at one point, we had the worst air quality in the world). Friends in group chats were voicing their immediate discomfort from the soot and dust — hacking coughs, itchy eyes, queasy nausea. What they missed were the longer term effects of pollution — increased asthma, bronchitis, heart failure — that disproportionately affect already underserved communities.
The cause of Smog-geddon NYC 2023 was smoke from wildfires up north that had drifted over, an increasingly frequent event as our planet warms up, heating our atmosphere and drying out vegetation. And it illustrates a topic I’ve been making sense of over the past few months: climate change and our health. The climate crisis is our most existential health crisis, and the U.S. healthcare industry is an outsized and overlooked contributor to our climate woes…
Why aren’t we — as startup builders, corporate leaders, and investors — talking about it more, let alone putting our “innovator” hats on to find new solutions to these big thorny problems?
I’m here to share my learnings going down the rabbit hole, on why we need to accelerate climate action in healthcare. This post covers:
- The compounding problem: Climate change and our health
- What we can be doing to accelerate climate action in healthcare
- Why now: Money, regulation, and stakeholder pressure
- Whitespaces for climate X health solutions
- Starting a conversation
The compounding problem: Climate change and our health
The ginormous problems — and opportunities — at the nexus of healthcare and climate change are best exemplified by the framework below, courtesy of my physician-innovator friend Chethan Sarabu and Sharon Lee:
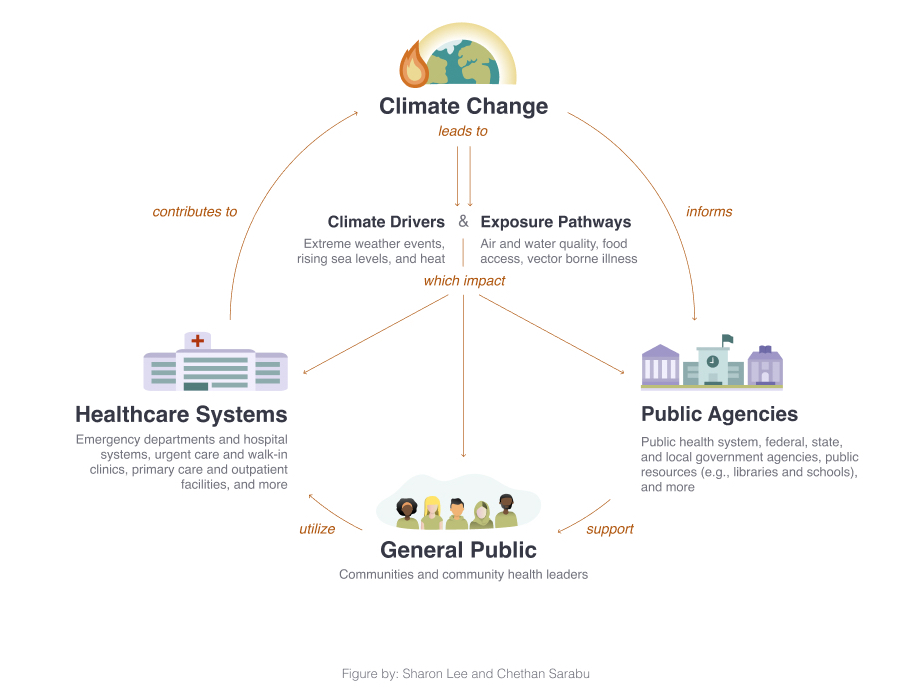
And it can be further simplified into two buckets: adaptation and mitigation.
Adaptation: How our climate impacts our health
Climate change has drastic impacts on our individual health, through social determinants like clean air, safe drinking water, food and shelter. Rising temperatures have led to an increase in vector-borne diseases, respiratory illnesses, heat-related illnesses… the list goes on.
Americans are experiencing it today. Thousands of children die prematurely each year from lower respiratory infections caused by air pollution from burning fossil fuels. With warming temperatures, the increased geographic range for ticks has led to a doubling of Lyme disease cases since 2000. As I’m typing this up at my local coffee shop patio, my sneezes are a testament to the increased pollen counts and worsened allergies. And if you were to put a price tag on it, the NRDC estimates the health costs of air pollution and climate change far exceed $800 billion per year.
As we get sicker, climate change is disrupting access to healthcare services. A majority of health systems have been affected by climate-related events such as wildfires or hurricanes over the past five years, with one health system citing $22 million in damages following a single extreme weather event. Unfortunately, the irony is that already underserved and marginalized communities — people of color, rural communities, historically redlined neighborhoods — are the least equipped to recover from climate change.
Working towards an equitable and accessible healthcare sector that betters our individual health means adapting to our changing climate.
Mitigation: How our health impacts our climate
But where does greenhouse gas (GHG) emissions, the cause of climate change, come from? Turns out, a big chunk comes from the U.S. healthcare sector.
For those who’re just starting their climate journey, let’s start with a primer on how GHG emissions are calculated. Globally, the agreed-upon standard for how orgs measure emissions is set by the Greenhouse Gas Protocol, which categorizes emissions into three scopes. Let’s apply the scopes to a health system’s emissions:
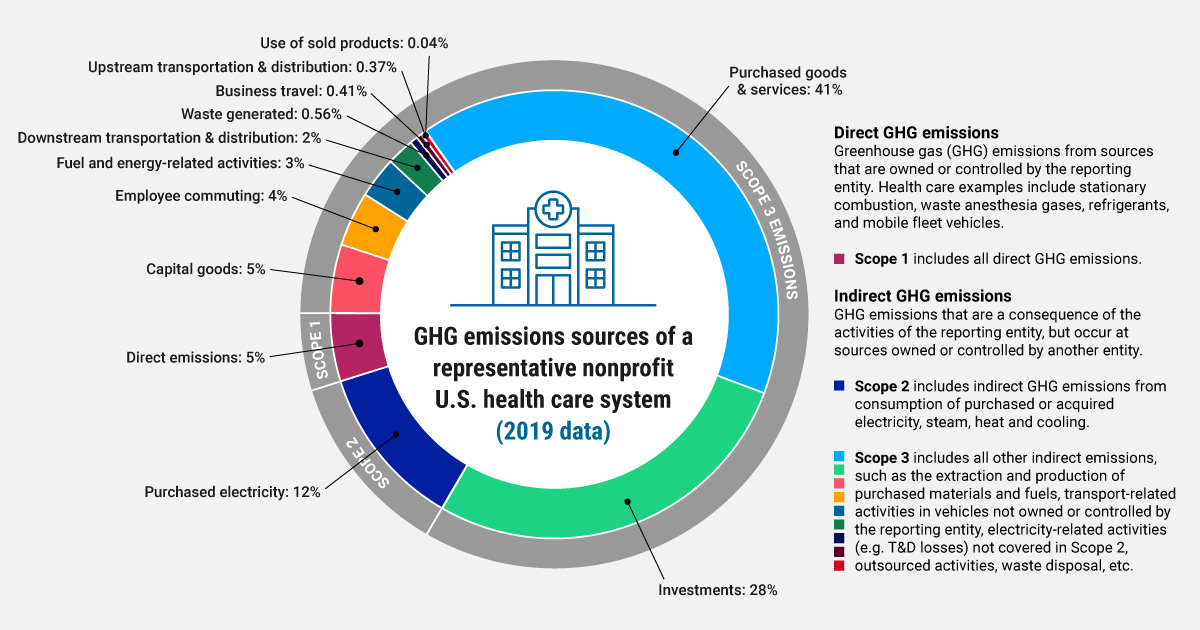
- Scope 1 are direct emissions from healthcare facilities, such as on-site boilers and certain medical gases,
- Scope 2 are indirect emissions through purchased electricity, and
- Scope 3 are indirect emissions across the supply chain and other sources (often dubbed “the iceberg beneath the surface" since it makes up ~80% of emissions)
Our $4.1 trillion healthcare sector (that’s 18.3% of our GDP) accounts for 10% of emissions in the U.S. That’s across health systems, clinics, payers, medical suppliers, biopharmas, and public health departments. We can have an outsized impact on the economy by using our healthcare sector’s purchasing power to drive the transition to clean energy and a low-carbon supply chain across the country.
Zooming out globally, while our healthcare system treats just 4% of the world’s population, it’s the most polluting system in the world accounting for 27% of all healthcare emissions worldwide. Decarbonizing the U.S. healthcare sector would also be a huge driver for decarbonizing globally.
Solving for climate change won’t happen without decarbonizing our healthcare sector.
What we can be doing to accelerate climate action in healthcare
To quote Michael E. Porter (of our favorite consulting framework), “The effects of climate change on companies’ operations are now so tangible and certain that the issue is best addressed with the tools of the strategist, not the philanthropist.” So much so, that the tools to combat climate change represent $75 trillion in business opportunities in the coming years!
I see startup builders, corporate leaders, and investors playing three main roles:
- Bringing existing ClimateTech solutions to healthcare. There’s tons of investments happening in ClimateTech (in fact, it seems recession proof, raking in $70.1 billion in venture funding last year). But if you look to the unicorns being built in carbon accounting and energy transition, they’re mainly selling into “sexy” sectors like finance, retail and tech. We need to help ClimateTech companies cross the go-to-market chasm into healthcare.
- Baking climate action into every healthcare company, to help leaders actively prepare for and mitigate their emissions. Healthcare leaders, who’ve been rapidly making climate commitments (see Why now), should have emission reduction targets embedded into their company’s strategy, operations, and culture.
- Creating new solutions purpose-built for healthcare. Climate solutions need to be built for their customers’ unique value chains. In healthcare’s complex value chain lies unique opportunities, like reducing emissions from medical gases and the hydrofluorocarbons in inhalers. Turns out, these gases are much more potent GHGs than carbon dioxide. Given that speed of execution is needed to meet climate goals and is a startup’s bread and butter, I’m stoked to champion founders journeying down this path.
Now, if you’re a cynic like me, you’re thinking, our healthcare sector’s still reeling from the aftermaths of COVID-19 and has bigger fish to fry in its quest to innovate. The business case for a healthcare org is driving financial and patient health outcomes; not our planet’s health.
My lightbulb moment was realizing that the climate opportunity is, in fact, in line with a healthcare org’s business case. In fact, it supports it. When you look at the principles for sustainable healthcare, it maps neatly into the overarching goals of a healthcare org, dubbed the “Quadruple Aim”):
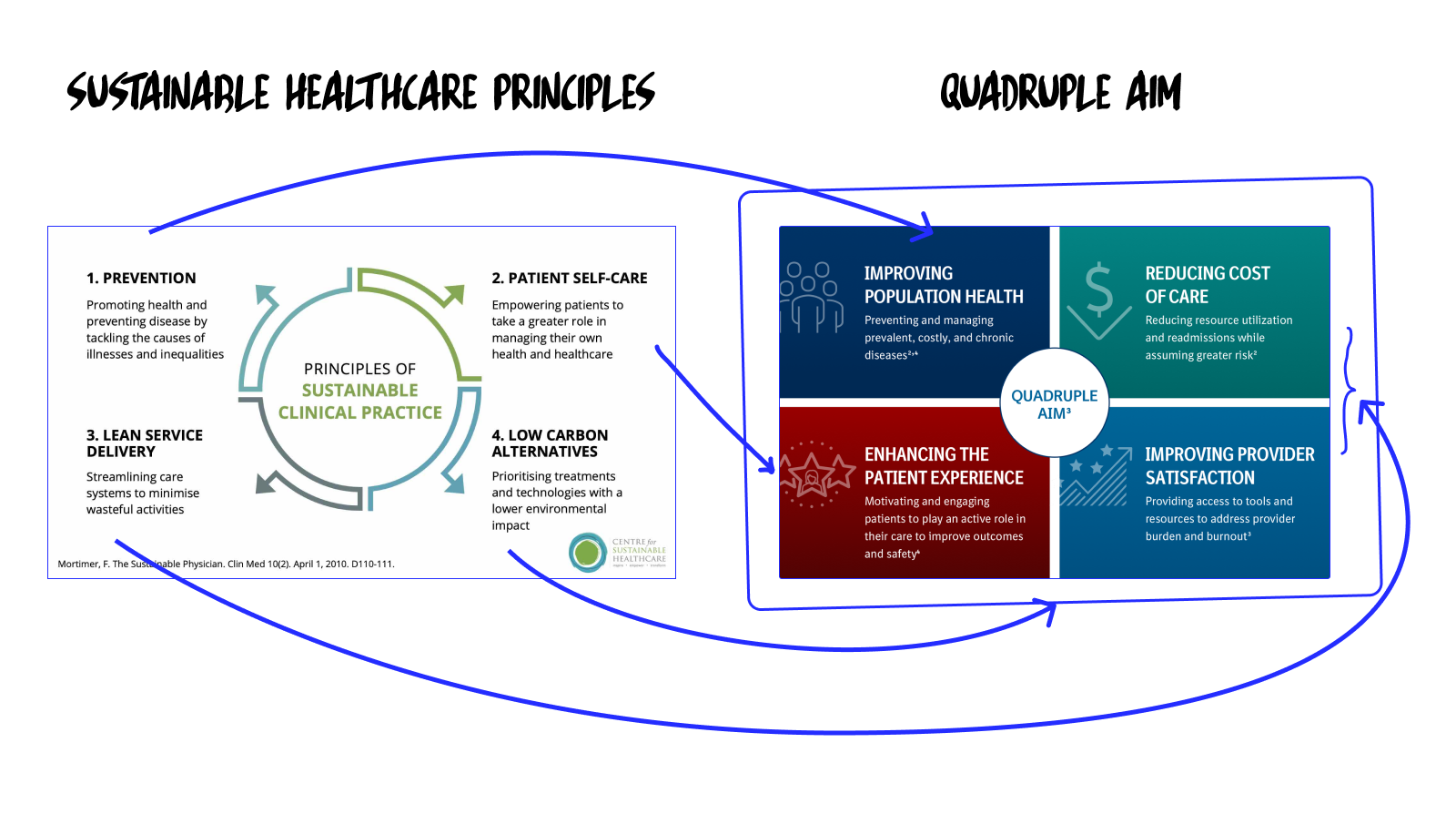
Instead of thinking about climate action in healthcare as its own separate problem to solve for, we should be reframing it as helping accelerate the existing clinical and financial goals of healthcare orgs.
Why now: Money, regulation, and stakeholder pressure
There’s three things that get an org to take climate seriously: (a) financial incentives, (b) sector-level regulatory requirements, (c) stakeholder pressure. The healthcare sector is feeling the heat on all three.
A. Financial incentives
Governments are pushing orgs towards energy reduction by providing tax incentives, loans, and grants. Under Biden’s Inflation Reducation Act, hospitals are able to tap into the single largest U.S. investment in climate and energy, including $250 billion to switching over to clean energy. And states have also been rolling out their own incentive programs.
Where governments have yet to formalize incentives, healthcare orgs are voluntarily filling in the gaps. One progressive health system I talked to tied exec bonuses to hitting certain GHG reduction targets.
B. Sector-level regulatory requirements
Commitments are finally happening in droves. 100+ healthcare orgs representing 800+ hospitals have signed on to a White House and HHS initiative for orgs to halve GHG emissions by 2030 and reach net zero by 2050. And you know the government is serious when they form an entirely new office, the Office of Climate Change and Health Equity, with its whole mandate being to help decarbonize the health care industry.
To help orgs meet those commitments, the Joint Commission, the nation’s oldest and largest standards-setting and accrediting body, is coming out with stringent environmental standards next month. While currently positioned as recommendations, orgs should be reading the tea leaves that environmental regulations tied to funding will become mandatory in the near future.
C. Stakeholder pressure
Respected non-profits and governmental agencies like Healthcare Without Harm, the Agency for Healthcare Research and Quality, and the National Academy of Medicine, are putting pressure on healthcare leadership. Around 90% of execs surveyed said that implementing climate mitigation and resilience strategies was an important priority.
Bottom-up, healthcare professionals are finding scrappy, clever ways to reduce the footprints of their own pathways while holding employers accountable. Anaesthesiologists are making the case to switch from desflurane to sevoflurane in the OR, an alternative anaesthetic gas that is 20 times less potent as a GHG. Facilities managers are implementing recycling programs to sustainably dispose of medical plastics, which make up 25% of all hospital waste. And professors are embedding climate change’s impact on health into the academic curriculum.
Whitespaces for climate X health solutions
If you’ve made it this far, I hope your mind’s flitting to solutions.
I wish I had a crystal ball. Instead, I have six whitespaces where I see impactful software and hardware solutions being applied or built:
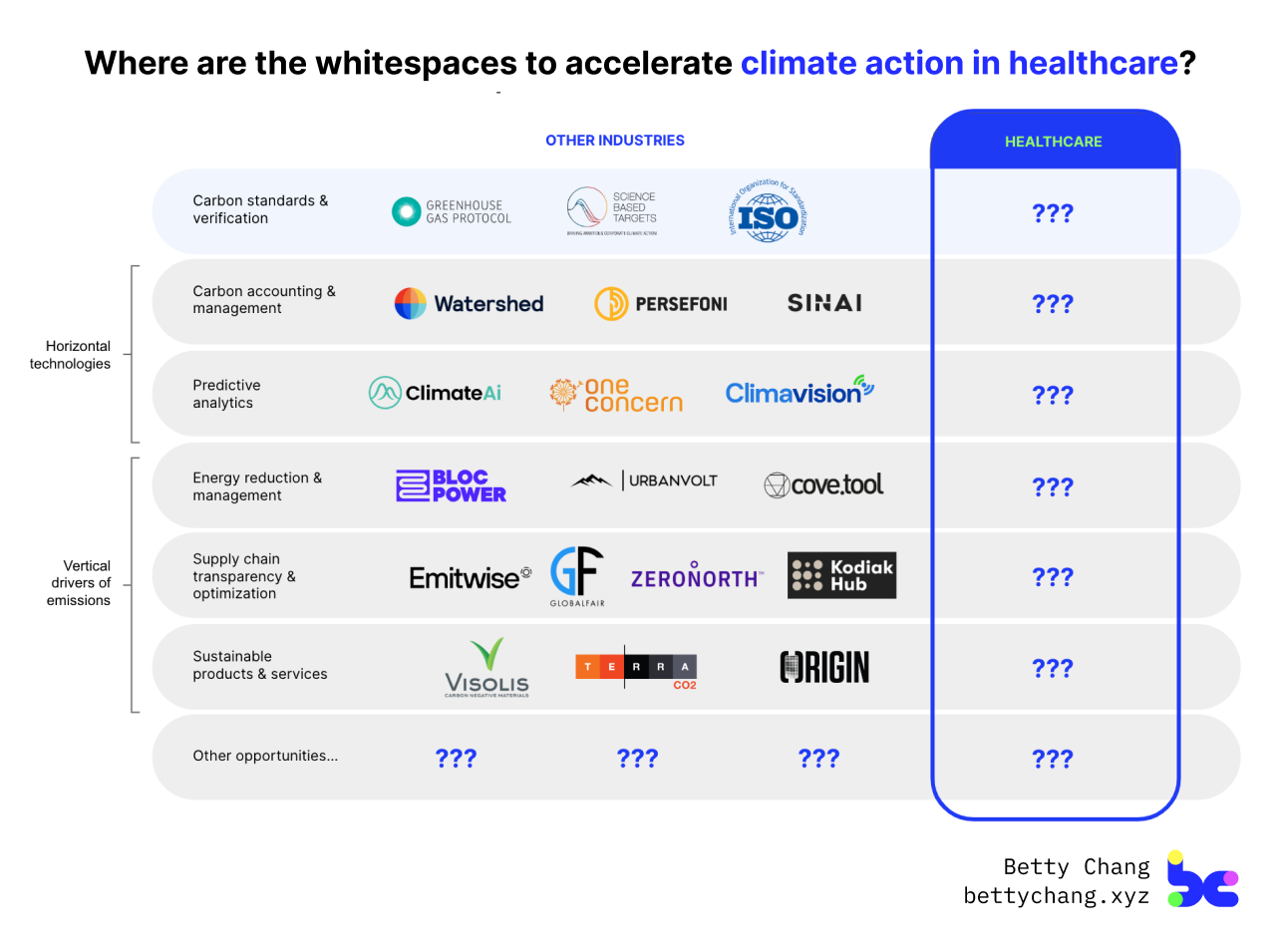
Opportunity #1: How can we help healthcare orgs account for and report on their GHG emissions?
To commit to science-based targets and track progress towards them, healthcare orgs need to be able to calculate their emissions across their organization. It’s not negotiable. Carbon accounting is the catalyst to a cascading of decarbonization strategies.
The global carbon accounting software market is worth $12.7 billion with verticalized incumbents staking their claim: Watershed serves tech companies, Persefoni has become the darling of financial firms, and CarbonCloud leads in the food sector. Yet, there’s no solution that’s designed for the healthcare value chain, including Scope 3 emissions which are the largest and most difficult to quantify.
A case study: A health system I spoke with had the most sophisticated carbon accounting solution… in Excel. They spent 3+ years building it from scratch because “no off-the-shelf tools exist,” integrating datasets across their EHR and account payables, generating heatmaps and visualization, and surfacing recommended actions. If you added up all the hours and resources that internal team members put in, it’d be a $1million+ project to create, let alone maintain. Imagine the savings and standardization from purchasing an off-the-shelf carbon accounting software, built for healthcare.
Opportunity #2: How can we better predict for how climate-related events impact care delivery and our individual health?
In a single year, ten climate-related events were estimated to cost the U.S. $10 billion. That includes costs associated with 900 deaths, 20,000 hospitalizations, 18,000 emergency room visits, and countless supply chain disruptions.
Predictive analytics solutions — which raised $267 million in funding last year — have big potential to help healthcare orgs build resilience by forecasting for future trends and scenarios, assessing and managing risk, and making better decisions. There’s abundant datasets and AI/ML advancements that can help public health departments prepare for the next outbreaks, procurement and emergency preparedness leads forecast for the next disruptions, and facilities managers plan for their next capital investments. but currently, environmental health data, healthcare system data, and public health data all live in separate, siloed systems.
A case study: The City of Boston developed a model that can be used to simulate the impact of different storm events on Boston’s stormwater system, to identify areas that are most vulnerable to flooding and develop strategies to mitigate those risks. This model takes from hard-won lessons of other cities like New York, that faced $3.1 billion in healthcare damages due to flooding from Hurricane Sandy… four hospitals’ ER and inpatient operations had to shut down for over a month.
Opportunity #3: How can we reduce energy use and transition to clean energy in our healthcare facilities, while maximizing financial incentives to do so?
Healthcare orgs provide intensive 24/7 services, consuming 10% of the total energy used in U.S. commercial buildings and spending more than $8 billion on energy every year. Hospitals consume 2.5x as much energy as office buildings and emit 2.5x as much carbon dioxide. And that’s not counting additional facilities like research labs, administrative offices, and satellite clinics.
Reducing energy use and transitioning to more efficient alternatives is low hanging fruit that directly impact Scope 1 and 2 emissions. Small fixes like upgrading lighting to more efficient LED fixtures and installing motion sensors to turn off lights in unoccupied areas go a long way. There’s also longer-term ROI projects of switching existing buildings to renewable energy sources that don’t rely on fossil fuels, and designing new construction sustainably from the ground up (the average hospital spends $10 million per year on new construction). The key is for orgs — especially critical hubs like FQHCs that serve the most vulnerable communities — to take advantage of incentives from the the IRA and state governments.
A case study: The Cleveland Clinic, which has 15 LEED certified buildings, has reduced its energy use intensity by 19%, leading to $50 million in savings. About one-third of the savings have come from small OR improvements. For example, reducing air changes (a mechanism used to keep the air clean) when ORs aren’t in use led to $2 million in savings a year.
Opportunity #4: How can we create a more transparent supply chain, to help procurement departments make smarter purchasing decisions?
When you break down where emissions come from in a health system, 60 to 80% are embedded in the products and services that we buy. Healthcare is one of the largest waste-producing sectors in the U.S., producing 6 million tonnes of waste annually. But the crazy part is that this waste is totally avoidable — $765 billion a year of medical supplies that are thrown out are in perfect, usable condition.
A health system’s supply chain makes up 40% of external spend, and it’s become a clear cost-savings priority for execs. Orgs could save billions per year by streamlining supply chain operations; for every $1 invested into optimizing the supply chain, a hospital could make $3 to $4 back.
Better procurement data is the backbone for a transparent supply chain — to avoid future disruptions, reduce waste, and improve margins. Upstream, procurement teams should be working with suppliers and GPOs to centralize medical supply data. Imagine a marketplace where you could easily compare and “shop” by price, specialty area, manufacturer reputation, and even the environmental impact of products. And downstream, teams can make more informed decisions by layering on clinician-level utilization data like type and frequency of purchases. I’ve got deep conviction that a unicorn is going to be built here in the next decade.
A case study: Kaiser Permanente implemented their Environmentally Preferable Purchasing (EPP) program and Scorecard to better evaluate and select products that do not contain harmful chemicals, while also encouraging suppliers to offer more sustainable supplies. In its first year, the program was estimated to save the org $26 million.
Opportunity #5: How can we figure out the environmental impact of healthcare products and services, and develop sustainable alternatives where needed?
A key ingredient to procuring sustainable products and services, is that these sustainable alternatives exist in the first place. There’s still tons of whitespace when it comes to measuring the environmental impact of healthcare products and services.
An obvious place to start is switching to sustainable packaging and eliminating single-used plastics. But there’s also the non-obvious R&D to validate what products and services are better for our planet: Does switching from in-person to telehealth visits or hospital-at-home models actually net out to less GHG emissions? What’s a lower-emission alternative to metered-dose inhalers? What’s the least potent anaesthetic gas, that’s still cost- and clinically-effective?
A case study: Eight Providence hospitals in Oregon switched from desflurane to sevoflurane as their primary anesthetic gas in the OR, after researchers showed that eight hours of using desflurane would be like driving a car for 1,600 miles, and that desflurane is 20x more potent as a GHG. The hospitals have seen a 95% drop in GHG emissions and cut anesthesia costs by 80%, given that sevoflurane is also way cheaper.
Continuing the conversation
I was at a friend’s birthday picnic in Central Park this weekend, and noticed the film of haze on the horizon. A check of the Weather app (now, an obsessive habit) showed the AQI was — again — “Unhealthy.” A scan of news headlines alerted me to a “killer heat wave” in Mexico, the “worst drought of the century” in Panama, and “off the chart ocean temperatures” in the North Atlantic. I couldn’t help wonder, if this was the new normal.
If you’re a fellow builder, investor or explorer, I hope this starts a conversation on how our health is impacted by climate change, and how our healthcare sector impacts our climate. And eventually we can turn conversation into (climate) action in healthcare.
I want to hear from you: What do you agree, or disagree, with? What opportunities do you see? What are you working on, and how can we help?
Shoot me an email or message me on Twitter.
Writing this post made me realize a big reason climate action in healthcare has been overlooked is that the sectors are individually complex to understand — so learning both becomes insanely complex. A big shoutout to my climate X health village for the learnings and feedback: Chethan Sarabu, Emily Mediate, Karen Ye, Nathan Eidelson, John Bogil.
